July 19, 2018
If you could do something to decrease stress, improve your body's ability to make vitamins, digest nutrients and decrease pain, would you? Our microbiome is ours to use or abuse, and it exists largely on the inside. Take a look at the shape of our digestive tract; the intestines are a twenty to twenty-five foot long tube lined with microvilli, the shag carpeting-like structure where digestion occurs. If you could flatten out the microvilli, the surface of our intestines would be the size of a tennis court. We need that much surface because there is so much activity in our intestines. Covering every inch are parts and pieces of the microbiome (bacteria, yeasts, fungi and viruses) packed in between the shags. The microbiome is a primary component of the immune system in the gut. Seventy percent of our entire immune system resides in the gut, and the microbiome comprises the majority of that system.
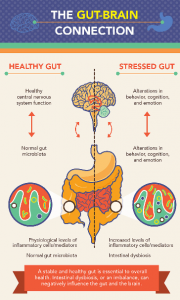
The microbiome is a community of bacteria, yeast and viruses that live in our guts, vaginal canals, nasal passages, mouths, throats, and on our skin. In the gut, it is critical for more than just digesting food; it is the control center for the whole body. The microbiome is linked to making vitamins, regulating metabolism and blood sugar and influences gene expression and brain chemistry. To exemplify this: for every message from the brain to the gut there are nine messages from the gut to the brain! Furthermore, your microbiome can weigh up to 5 pounds, nearly twice as much as our brains! There are 100 to 150 times more genes in our microbiome than the 23,000 genes in human DNA. There are 10X more cells of bacteria in our gut than all the cells in the rest of the body put together. Because of this, many experts have come to think of the microbiome as less like an additional organ in the body and more like a completely different organism, with a life of its own. For more information on the microbiome check out Dr. Tom O'Bryan's book The Autoimmune Fix at theDr.com.
If a web search is done with just the search words microbiome and pelvis, 6 pages of results pop up! Scientists are trying to get to the bottom of the cause of pelvic pain and have drawn correlations between people with IC, overactive bladder, male and female pelvic pain, depression and anxiety and how their microbiomes are different from healthy controls. The reason this could be so impactful is that changes in the microbiome can have impact on sensitivity of the nerve endings that cause pain.
We are just hitting the tip of the iceberg with research in this area. Even in the infancy of research, one thing has been established; there is a statistically different microbiome in patients with just about any type of pelvic disorder compared with controls. This imbalance means there are higher levels of some bacteria and viruses and lower numbers of others, this is a term called dysbiosis. For the most part, I tell my patients that altered gut flora has been found to be detrimental to all kinds of pelvic issues.
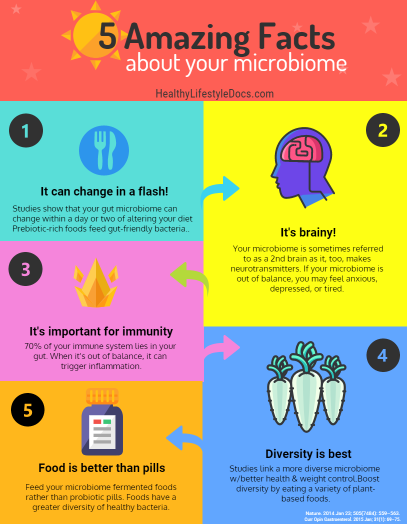
Dr. DJ Klumpp suggests we should look toward therapy through mechanistic probiotics. Other researchers at this point are saying there is some evidence to supplement with lactobacillus probiotics. They see a particular decrease in the bacteria lactobacillus, which is why they are recommending probiotics with lactobacillus. That seems like a good idea on the surface, but a better plan is to improve your habitat for this amazing organism. It seems daunting because there are many factors at play, but decreasing stress is one way to make the microbiota thrive, oftentimes creating a positive feedback loop. Altered microbiota creates anxiety and increased stress, balanced microbiota creates decreased stress levels.
So, what are we to do when we are sick, stressed out and in pain? Make our insides hospitable to the microbiome by changing what we put into our mouths. In Dr. Mark Hyman's book, Food – What the Heck should I Eat? he describes the why's, and what to eat to clean up our diet so we can thrive. Here are a couple of hints regarding cleaning up our body to be more hospitable to the good bacteria, fungi and viruses that inhabit or no longer inhabit our guts.